Understanding IVF: A Comprehensive Guide
Introduction to IVF
In vitro fertilization (IVF) is a widely recognized assisted reproductive technology that has brought hope to countless couples facing fertility challenges. Since its inception, IVF has evolved significantly, offering a viable solution for individuals and couples who struggle to conceive naturally. The importance of IVF lies not only in its ability to assist in conception but also in its role in advancing reproductive medicine and providing insights into human fertility.
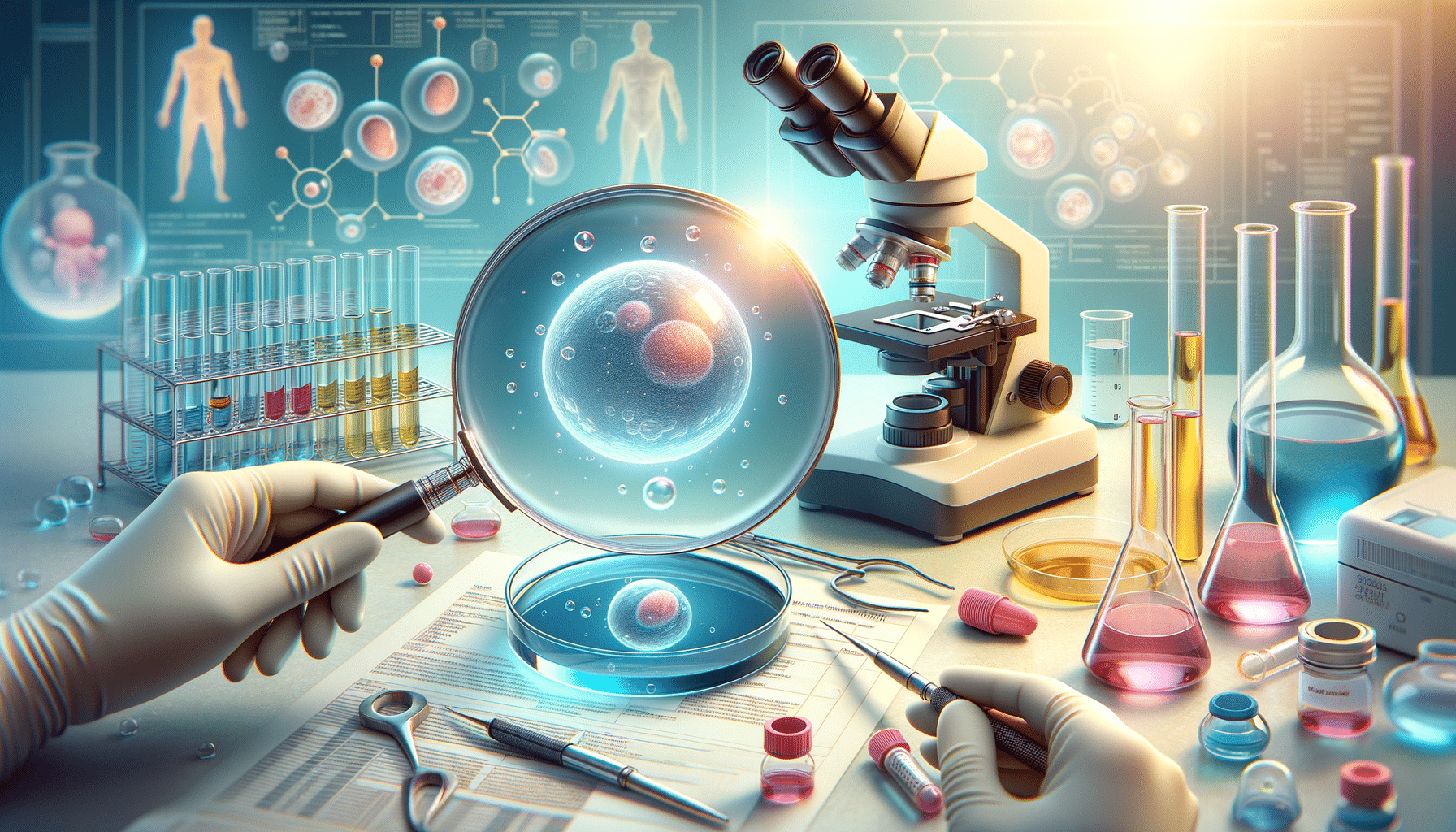
IVF involves retrieving eggs from a woman’s ovaries and fertilizing them with sperm in a laboratory setting. The fertilized egg, or embryo, is then implanted into the woman’s uterus. This process bypasses several potential barriers to conception, such as blocked fallopian tubes or low sperm count, making it a crucial option for many facing infertility.
The IVF Process: Step by Step
The IVF process is intricate and involves several steps that require careful coordination and medical expertise. Here’s a breakdown of the typical stages involved:
- Ovarian Stimulation: The process begins with hormone injections to stimulate the ovaries to produce multiple eggs. This increases the chances of retrieving viable eggs for fertilization.
- Egg Retrieval: Once the eggs are mature, they are retrieved through a minor surgical procedure called follicular aspiration. This is usually done under sedation to ensure comfort.
- Fertilization: The retrieved eggs are then mixed with sperm in a laboratory dish. Fertilization can occur naturally or through intracytoplasmic sperm injection (ICSI), where a single sperm is injected directly into an egg.
- Embryo Culture: Fertilized eggs, now embryos, are cultured in a controlled environment for several days. During this time, they are monitored for development and quality.
- Embryo Transfer: One or more healthy embryos are selected and transferred into the uterus. This is a simple procedure that does not require anesthesia.
The success of IVF can depend on various factors, including the age of the woman, the quality of the eggs and sperm, and the specific cause of infertility. It’s important for couples to have realistic expectations and to discuss potential outcomes with their healthcare provider.
Benefits and Considerations of IVF
IVF offers numerous benefits, making it a valuable option for many people. Some of the key advantages include:
- Overcoming Infertility: IVF can address various infertility issues, including blocked fallopian tubes, male factor infertility, and unexplained infertility.
- Genetic Screening: IVF allows for preimplantation genetic testing, which can help identify genetic disorders and select embryos without genetic abnormalities.
- Control Over Timing: IVF enables couples to plan the timing of their pregnancy, which can be particularly beneficial for those with demanding careers or personal commitments.
However, there are also important considerations to keep in mind. IVF can be emotionally and physically demanding, requiring a significant commitment of time and resources. The financial cost can be substantial, and not all insurance plans cover IVF treatments. Additionally, there are potential risks associated with the procedure, such as ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies.
Prospective parents should weigh these factors carefully and consult with fertility specialists to make informed decisions that align with their personal circumstances and goals.
IVF Success Rates and Factors Affecting Outcomes
Understanding the success rates of IVF is crucial for couples considering this option. Success rates can vary based on several factors, including:
- Age: The age of the woman undergoing IVF is one of the most significant factors. Younger women typically have higher success rates due to better egg quality.
- Cause of Infertility: The underlying cause of infertility can impact the likelihood of success. For instance, IVF may be more successful in cases of tubal factor infertility compared to severe male factor infertility.
- Embryo Quality: The quality of the embryos, as assessed by embryologists, plays a crucial role in determining the chances of a successful pregnancy.
- Clinic Experience: The expertise and experience of the fertility clinic and its staff can influence outcomes. Choosing a reputable clinic with a strong track record is essential.
According to recent data, the average success rate for IVF is around 40% for women under 35, with rates decreasing with age. It’s important for couples to discuss individual prognosis with their healthcare provider to understand what they can realistically expect.
Future of IVF: Innovations and Ethical Considerations
The field of IVF continues to evolve, with ongoing research and technological advancements paving the way for improved outcomes and expanded possibilities. Some of the exciting developments include:
- Improved Genetic Testing: Advances in genetic testing are enabling more comprehensive screening for genetic disorders, increasing the likelihood of healthy pregnancies.
- Artificial Intelligence: AI is being used to enhance embryo selection processes, potentially increasing success rates by identifying the embryos with the highest potential for successful implantation.
- Personalized Medicine: Tailoring IVF protocols to individual patients based on genetic and biological factors is becoming increasingly feasible, offering more personalized and effective treatment options.
Alongside these innovations, ethical considerations continue to be a topic of discussion. Issues such as the ethical implications of genetic selection, the use of donor gametes, and the potential for creating “designer babies” are important conversations that society must navigate as technology progresses.
Overall, the future of IVF is promising, with the potential to bring hope and new possibilities to those seeking to build their families.